The FDA Is Coming for Your Natural Thyroid Meds

If you're one of the millions who swear by Armour Thyroid or NP Thyroid because synthetic levothyroxine left you feeling like a zombie, you should know the FDA just moved to reclassify these natural desiccated thyroid (NDT) medications as "biologics." That sounds benign until you realize manufacturers now need to submit entirely new drug applications—by a 2026 deadline—or face removal from the market.
The timing is revealing. NDT medications have been used since the 1890s, long before the FDA existed. They were "grandfathered" in precisely because they had a century-long track record. Now the agency wants modern trials, modern manufacturing oversight, and modern prices. For patients who've spent years finding a medication that actually works, this isn't regulatory housekeeping—it's an existential threat to their treatment protocol.
The practical reality: Patients currently stable on NDT may face significant access challenges. If you're on Armour or NP Thyroid, now is the time to have a backup conversation with your endocrinologist about synthetic alternatives—not because they're better, but because they might be your only option.
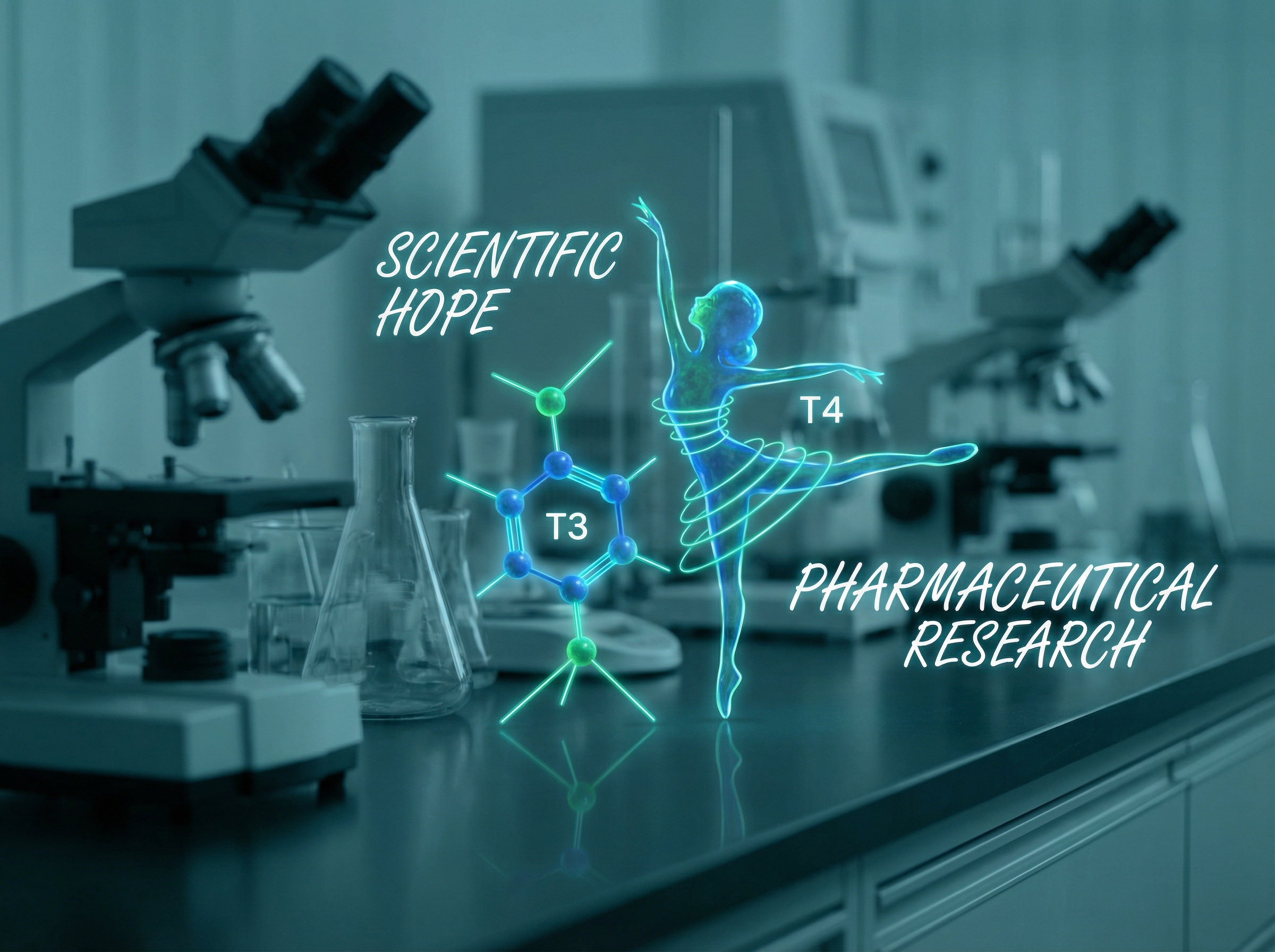
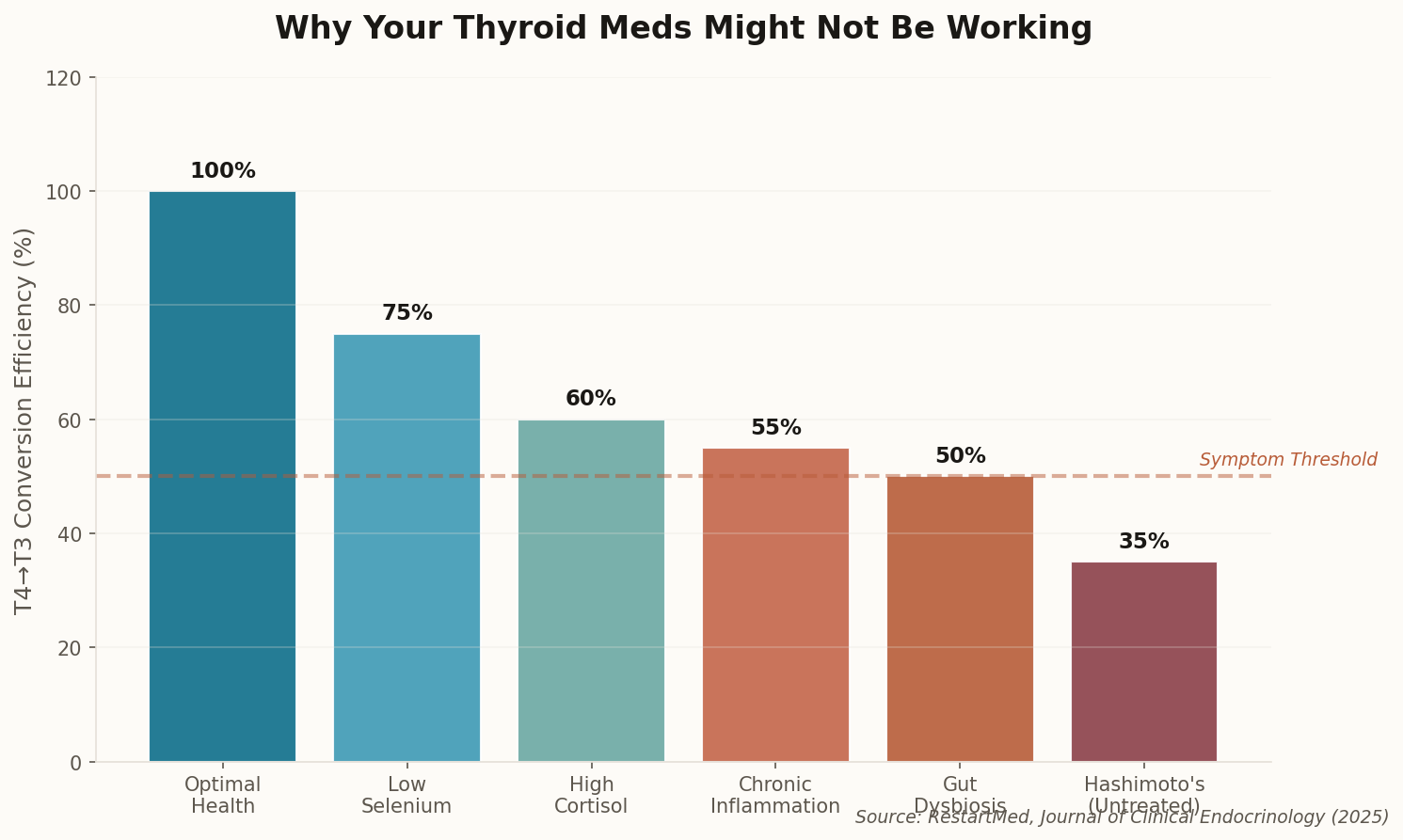
The larger issue here is that NDT works differently than synthetic T4. It contains both T4 and T3—the active hormone that your cells actually use. For the 15-20% of patients who can't efficiently convert T4 to T3, NDT isn't a lifestyle choice. It's the difference between functioning and not functioning. The FDA's move treats all patients as identical when the endocrine system is anything but.