The Acne Drug That May Be Stealing Your Bones

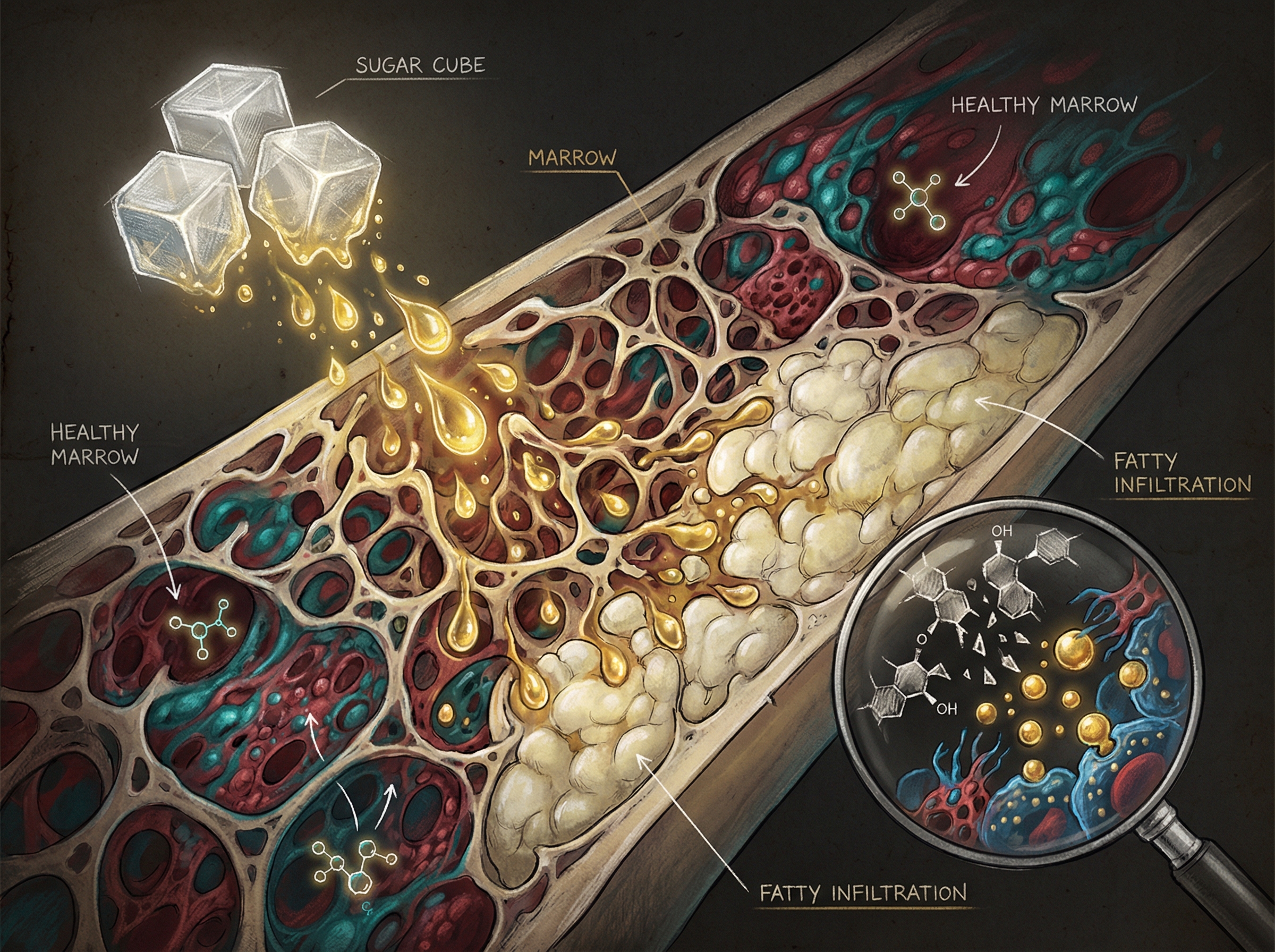
Here's a question that probably never came up in your dermatologist's office: What does clear skin cost your skeleton? A new systematic review and meta-analysis finds that isotretinoin—the nuclear option for severe acne, sold under brand names like Accutane and Absorica—may be quietly altering bone remodeling in ways that increase osteopenia risk.
The mechanism isn't mysterious. Isotretinoin is a vitamin A derivative, and vitamin A in excess is a known bone antagonist. What's new is the quantified correlation: patients on long-term isotretinoin therapy showed measurably decreased bone mineral density compared to controls. The effect was most pronounced in younger patients—exactly the demographic most likely to be prescribed it.
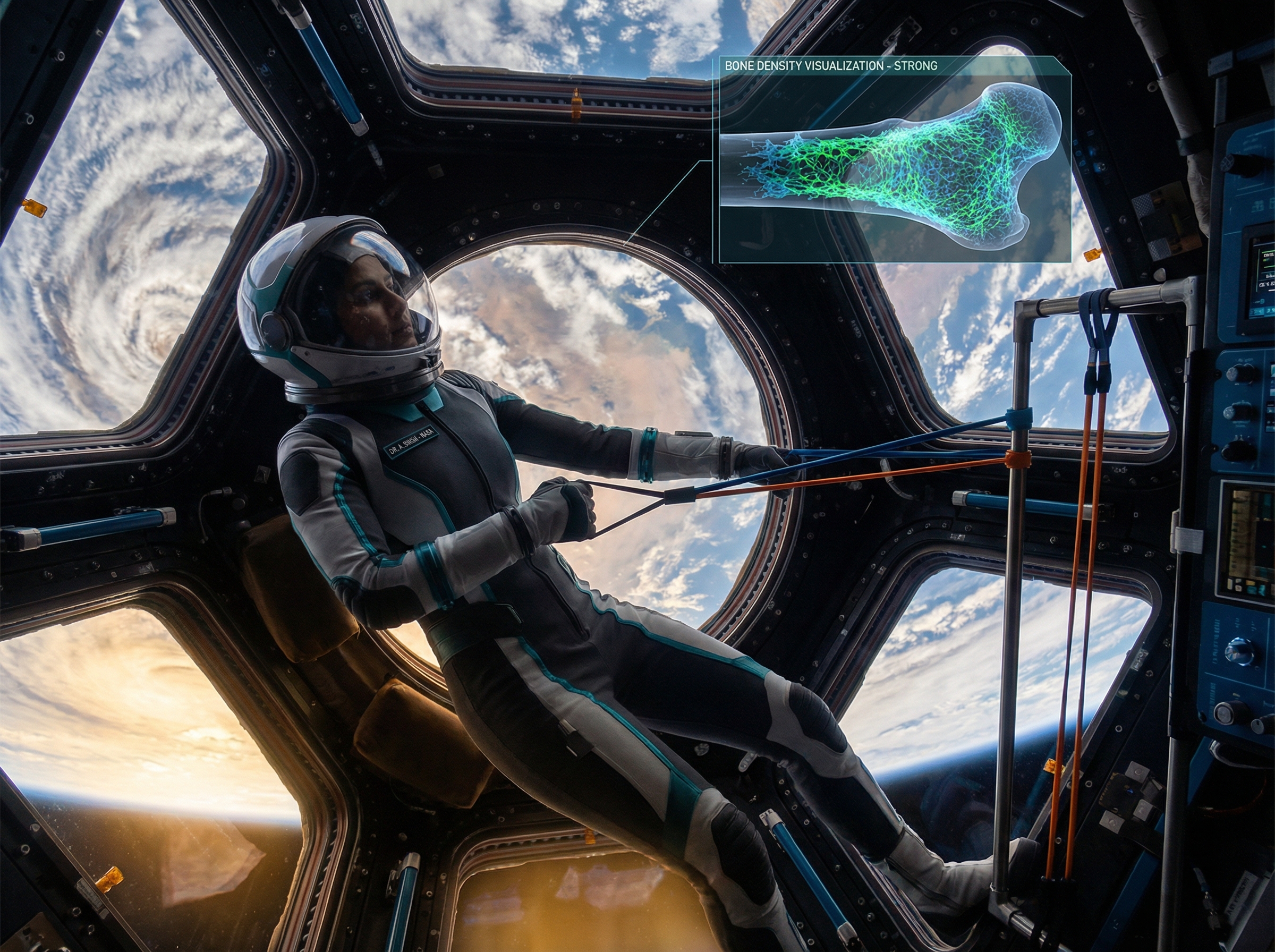
The clinical implication is straightforward but rarely practiced: if you're prescribing isotretinoin for more than a few months, bone health monitoring should probably be part of the protocol. For the millions who took it as teenagers and are now hitting their 40s, this is another variable to consider when your doctor mentions "age-related bone loss." It might not be entirely about age.