Six in Ten Adults Are Sleeping Poorly. Now We Have the Numbers.
When researchers talk about "sleep debt," it often sounds like metaphor. A study released today makes it viscerally concrete: 60.3% of adults in a large population-based cohort are sleeping poorly. Not occasionally tired—clinically defined poor sleep quality, the kind that accumulates into chronic disease.
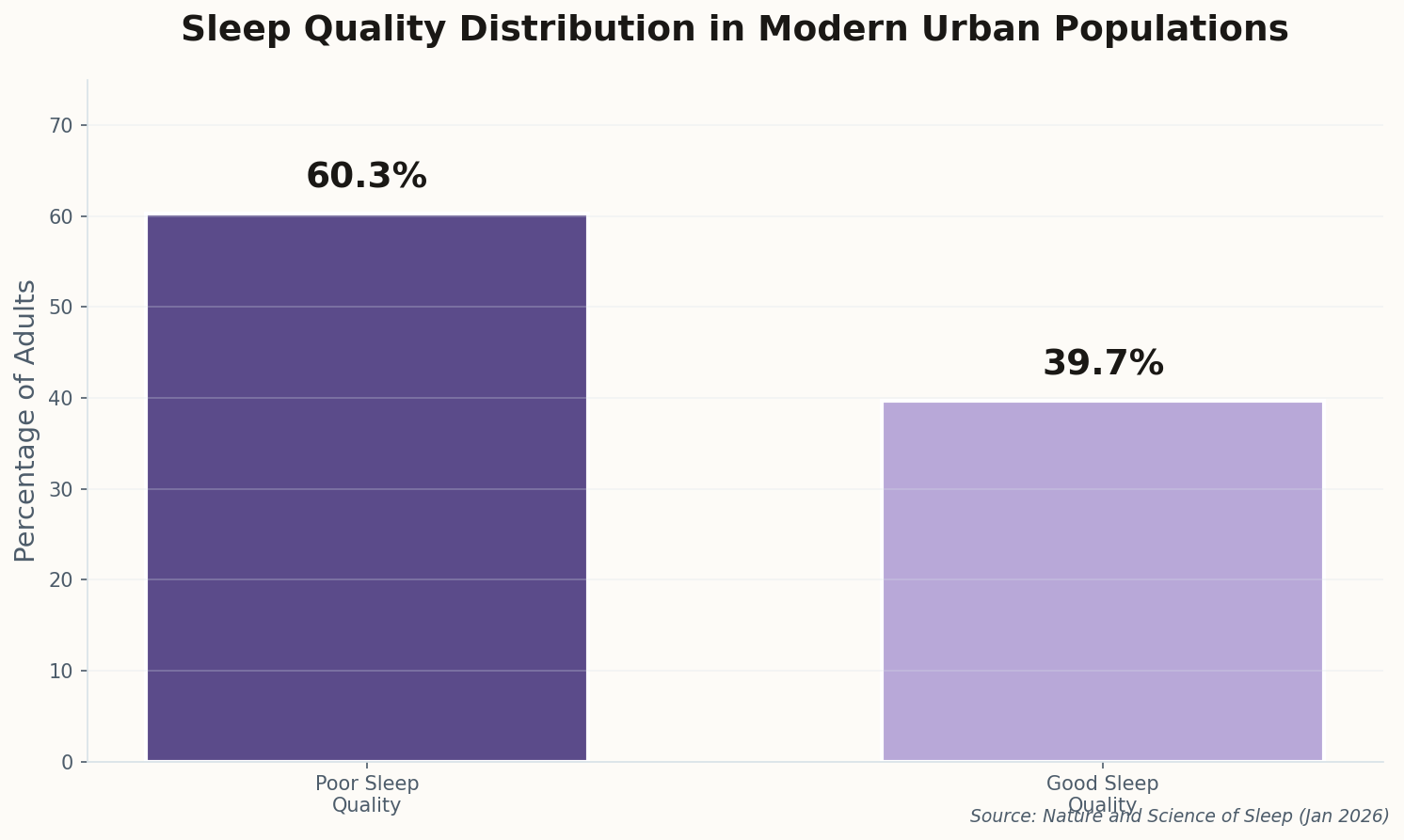
The study, conducted in Qatar, identified three independent drivers: smoking, high perceived stress, and poor sleep hygiene. What makes this significant isn't the surprise—we knew these factors mattered. It's the scale. In a rapidly modernizing, high-income country with excellent healthcare access, six in ten adults still can't sleep properly.
This isn't a developing-world infrastructure problem. It's a modernity problem. The same stress patterns, screen habits, and work pressures exist in New York, London, and Singapore. The paper's authors called for "targeted public health interventions," but what does that actually look like? Telling stressed professionals to put down their phones hasn't worked particularly well so far.
The uncomfortable implication: Sleep is the canary in the coal mine for modern life. We've optimized everything except our ability to shut down.