Selenium Finally Gets Its Due: Major Meta-Analysis Confirms Antibody Reduction
For years, selenium supplementation lived in a gray zone between "promising" and "prove it." That era is over. A comprehensive systematic review and network meta-analysis has confirmed what many functional medicine practitioners suspected: selenium significantly reduces both TPOAb and TgAb levels in Hashimoto's patients.
The data is unambiguous. Patients showed measurable antibody reduction regardless of whether they were already on levothyroxine replacement. Even more compelling: the analysis highlighted selenium's role in reducing oxidative stress markers, specifically malondialdehyde. This suggests we're not just masking symptoms but addressing underlying inflammatory mechanisms.
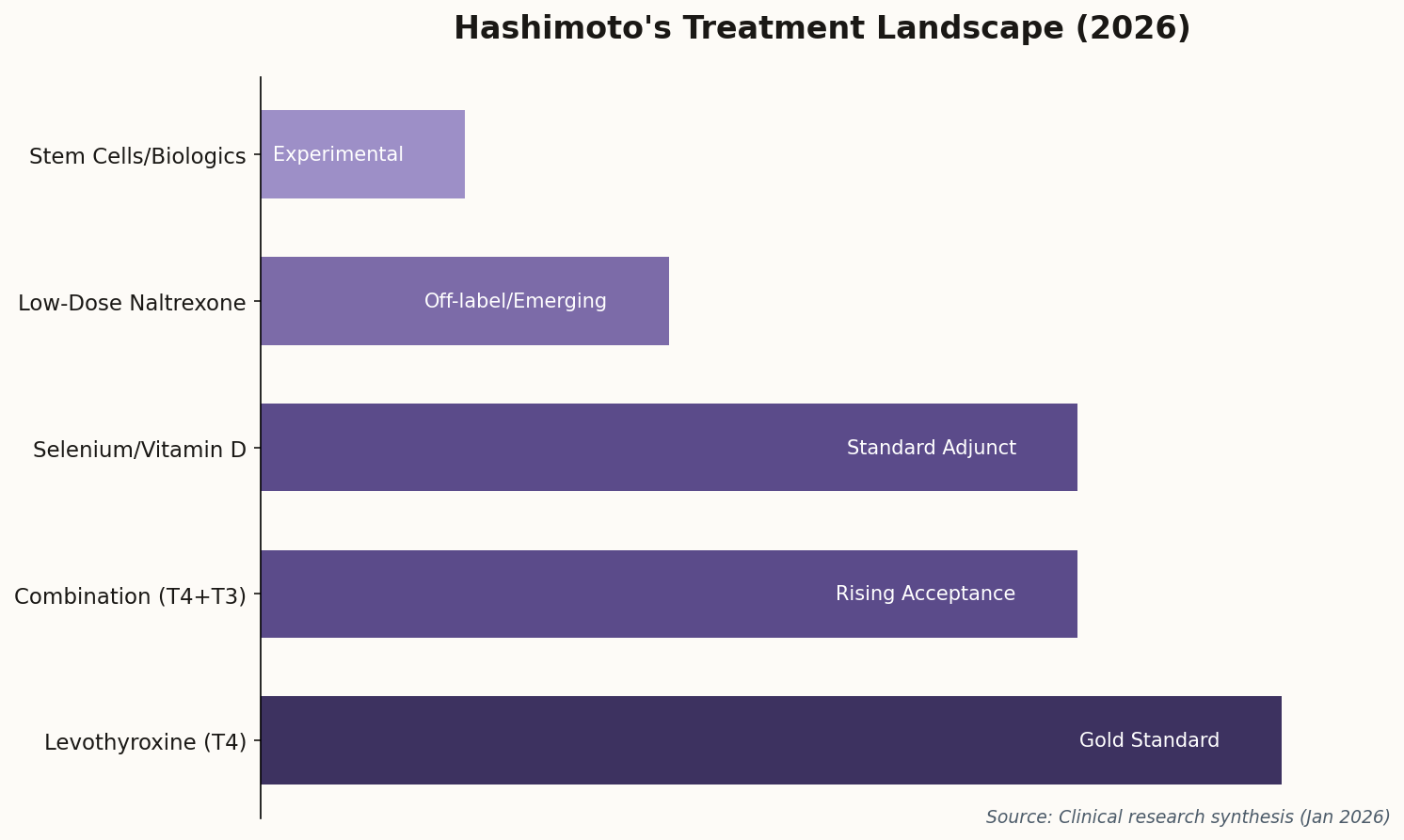
The clinical implication: Selenium supplementation has graduated from "experimental" to "evidence-based" for antibody reduction. If your endocrinologist hasn't discussed it, bring it up.
The standard dosage in these studies: 200mcg daily. But here's the critical nuance most coverage misses: selenium has a narrow therapeutic window. More is not better. Toxicity symptoms can emerge at doses only 2-3x the beneficial amount. This is precisely why medical supervision matters.